Main Pillars of Research in Revolutionary Geroscience Field
Summary: Exploration of the main pillars of research in the field of longevity science, the 2nd installment in a continuation of the 4-part essay titled Geroscience by Felipe Sierra. [With an introduction by Brady Hartman. ]
Scientists in the emerging field of geroscience have significantly slowed down aging in laboratory animals and aim to the same thing for humans.
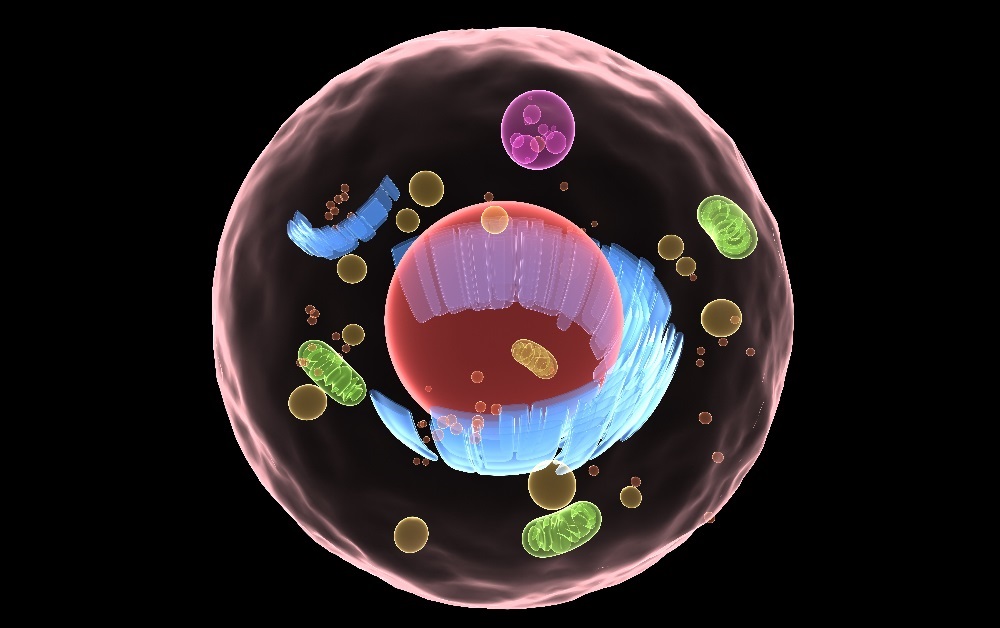
This is a continuation of the essay Geroscience by Felipe Sierra, Ph.D. In this segment, ‘The Main Pillars of Research on Aging Biology, Dr. Sierra shows us how longevity researchers, called geroscientists, are trying to manipulate the underlying biology of aging by understanding the hallmarks of aging, which consists of factors such as inflammation, responsiveness to stress, epigenetic changes, a change in metabolism, the build-up of macromolecular damage, loss of proteostasis, and stem cell decline
Felipe Sierra, Ph.D. is leading the U.S. government’s geroscience efforts, who are looking into why we age, and how to slow it down. Dr. Sierra is the Director of the Division of Aging Biology at the National Institute on Aging (NIA). The emerging field of geroscience is populated by geroscientists, a new type of researcher who aims to understand aging to develop treatments that slow or reverse the aging process.
The Main Pillars of Research on Aging Biology
(from the article Geroscience by Felipe Sierra, Ph.D.
In October 2013, a group of experts convened in Bethesda, Maryland, to discuss the current status of research in geroscience, the intersection between basic aging research and chronic diseases. [15] Seven major areas were discussed, and these overlap significantly with the areas identified by López-Otín and colleagues in a recent opinion piece. [16] These represent apparent drivers of the process and will be the focus of this discussion. It should be mentioned, however, that we are still in dire need of markers that can be used for research purposes, independently of whether they are drivers or not. The field has traditionally shied away from looking at biomarkers under the assumption that markers of aging might be too elusive. However, new techniques, including a large set of -omics technologies, now open new possibilities that need to be explored; in the absence of such markers, progress in the field remains hindered. In addition to markers that can be used to test the effects of interventions, there is a need to define mechanistic drivers that can be targeted for these interventions, thus paving the way for possible therapeutics that might delay aging and concomitantly delay the onset and/or severity of multiple chronic diseases and conditions that affect primarily the older population.
Major areas currently considered as potential drivers of the aging process include inflammation, [17] responsiveness to stress, [18] epigenetics, [19] metabolism, [20] macromolecular damage, [21] proteostasis, [22] and stem cells. [23] A brief overview of each of these topics follows.
Inflammation
Inflammation is a crucial early response that allows the organism to defend itself against aggression by pathogens or tissue damage. Inflammation has been associated with multiple chronic diseases of older adults [19,24]; yet, due to its protective role, dampening it might have serious deleterious effects, and it is important to preserve this response, even into old age. The molecular and cellular mechanisms involved in the inflammatory response have been well studied in young organisms, and a proper response is swift and short-lived. Aged organisms also often mount a vigorous response to challenges; in fact, in some aspects, it is an exacerbated response [25-27]; however, in many cases, they fail to turn off the response properly, leading to a low-level inflammation termed sterile inflammation. [28] This is characterized by a mild chronic elevation in the serum levels of several cytokines and acute phase factors, some of which, such as interleukin 6 (IL-6), tumor necrosis factor-α (TNF-α), and C-reactive protein (CRP), are actively used in the clinical setting to assess inflammatory status. [29-31] This age-related, low-grade chronic inflammation might be a contributing factor to chronic diseases and conditions, and therefore efforts at curbing the inflammatory response are currently ongoing in the clinic. However, as mentioned earlier, interventions aimed at dampening the inflammatory response altogether (e.g., anti-inflammatories) might be ill-advised for two reasons: (1) the main defect with aging appears to be in the shutting-off phase; and (2) dampening the response would leave older adults susceptible to disease from pathogens and injury. It really needs to be clarified about whether sterile inflammation is really a maladaptive response before proceeding to the clinic. It is also entirely possible that the low-level inflammation is not really maladaptive, but might be an appropriate adaptive response to age- or disease-induced tissue damage or other injurious activities, such as changes in the microbiome and/or gut leakage. More focused research in this arena is needed.
Adaptation to Stress
In common parlance, stress refers primarily to psychological issues. In addition to the molecular underpinnings of psychological stress (e.g., cortisol), cells are also constantly exposed to stressors at the molecular level, including free radicals, environmental toxins, and UV light. Both types of stressors appear to accelerate the rate of aging, at least when they are chronic, [18,32] and recent work is beginning to show the interrelations between psychological stress and molecular responses, such as telomere shortening. [33-35] The similarities and differences between molecular and cellular responses to a variety of stresses have not been studied in detail, and it is possible, although still rather unproven, that the responses elicited by different sorts of stress might have commonalities at the subcellular level. If so, then the source of stress becomes less relevant, and a new focus on the mechanisms used by the cell to respond might become targets for future investigation. It might prove easier to intervene on the ability of the organism to respond to stress than to try to eliminate all sources of stress, something that is clearly unattainable. It has been observed that although powerful acute or mild chronic stresses are detrimental, [18,32] some mild stresses (both physiologic and psychological) appear to be beneficial, probably through a mechanism related to hormesis. [36] The mechanisms that control the switch between beneficial and detrimental are currently unknown, and they might relate to whether the stress is chronic or acute. Further understanding of this level of control could, in principle, allow researchers to manipulate that pivoting point in a manner that might allow us to increase the positive and decrease the negative.
Epigenetics
Efforts at understanding the genetic underpinnings of aging have been very fruitful in the past, and the discovery that individual genes and pathways can increase life span in many species was crucial in turning aging research from the descriptive to the mechanistic phase. Furthermore, some of the findings initially described in lower organisms (worms and flies) have been shown to correlate with extreme longevity in human populations (centenarians). [14] There has been a renewed interest in the epigenome, which is more malleable and might better reflect the role of additional modifiers of aging, including diet and the environment. In lower organisms, significant changes in the epigenome, including heterochromatin, transposable elements, and histone modifications, have been described to occur as a function of age. [37-40] Epigenetic changes have also been associated with a number of age-related diseases such as cancer [19] and, because aging is the major risk factor for most chronic conditions, including cancer, the cross-talk between epigenetic changes due to aging and those due to disease are being explored. Another active area of research, related to the previous section, “Adaptation to Stress,” is the resolution between beneficial and deleterious adaptations to stress, because epigenetic marks might integrate complex responses to the environment. Thus, it is important to establish to what extent these epigenetic changes can drive pathology and to what extent those changes might be reversible. The origin of epigenetic changes and their downstream effects are currently the subject of intense study.
Metabolism
Aging is associated with many metabolic changes, and a challenge for researchers is to identify those that are causative factors of aging and disease susceptibility and differentiate those that simply correlate and those that represent adaptive responses. Changes in metabolism have been associated with age-related diseases, including diabetes, cardiovascular, cancer, and neurodegenerative diseases. Although diabetes is considered primarily a metabolic disease, this is not the case for many others. Interestingly, many pathways that affect longevity have been shown to play critical roles in metabolism. This includes the first genetic pathway described as aging-related, the insulin-IGF pathway, as well as the mammalian target of rapamycin (mTOR) pathway. In addition, the best characterized way of extending life span, caloric restriction, should be considered primarily as a metabolic intervention. Sirtuins represent another pathway that affects aging, and it has also been shown to have dramatic effects on cellular metabolism, probably via regulation of NAD+ (nicotinamide adenine dinucleotide, oxidized form) levels. [41] Sirtuin activators such as resveratrol have been shown to extend life span in several species but, at least in mice, resveratrol only extends life span if the animals are maintained under the severe metabolic stress imposed by a very high-fat diet. [42-44] Mitochondria also represent a central hub in energy metabolism and have received considerable attention from researchers on aging. For a long time, the focus was on their role as potential sources of reactive oxygen species (ROS) and macromolecular damage [21,45] and, contrary to expectations, reducing the activity of the mitochondrial electron transport chain leads to increased longevity, perhaps because of reduced electron leakage, which results in reduced free radical production. [46-48] In addition to their role in producing free radicals, mitochondria have also been studied extensively because of their central role in intracellular energy production. In addition to these classical modifiers of metabolism, current interests include other factors, such as changes in the microbiome [49,50] and in circadian rhythms, [51,52] both of which have dramatic metabolic and proinflammatory effects.
Macromolecular Damage
The free radical theory of aging has been a major player in aging biology research for more than a half-century. [53] The original theory suggested that damage to macromolecules produced by free radicals in the mitochondria will result in the loss of cellular and tissue function observed during aging. Considerable circumstantial evidence in favor of that hypothesis has accumulated in the last few decades. However, a comprehensive attempt at testing this theory was provided in the form of a set of mouse models that were genetically manipulated to increase or decrease free radical scavenging capabilities. Most of these manipulations did lead to the expected changes in macromolecular damage (decrease or increase, depending on whether defenses were increased by transgenic technologies or decreased in knockout models) but, surprisingly, they did not affect mean or maximal life span. [45,54]
A notable exception is the MCAT (mitochondrial catalase) mouse model, where expression of catalase in the mitochondria (but not other subcellular compartments) leads to increased longevity and a decrease in cardiovascular disease. [55] In spite of these results, the free radical theory remains a stalwart of research, because free radical damage has been repeatedly correlated with various age-related diseases, including cancer and cardiovascular diseases, the main killers in the Western world. [56]
It seems likely that the negative results indicate that like resveratrol, free radicals only play a role in longevity under stressed conditions, but not under standard Institutional Animal Care and Use Committee (IACUC)–approved mouse housing. Importantly in that regard, controlling free radicals seems to play a role in health span, irrespective of their role in life span. In addition to protein damage, DNA damage driven by manipulation of mitochondrial or nuclear DNA repair systems do lead to phenotypes that some authors call “accelerated aging.”[57-59] In independent research studies, it has been found that many human accelerated aging syndromes, such as Hutchinson-Gilford, Werner, and Cockayne syndromes, the culprits for the disease have been identified as mutations in genes involved in DNA repair or other DNA transactions, including structural integrity of the nuclear lamina. [60,61] As discussed earlier (“Adaptation to Stress”), it is entirely possible that the apparent acceleration of aging phenotypes in these models and diseases might not be the direct result of DNA damage, but the phenotypes might be related to the cell’s response to that damage, leading to cell senescence, stem cell depletion, or other outcomes. [62] Finally, telomere integrity can also be considered as a subset of macromolecular damage, because there is evidence supporting the notion that telomere shortening leads to deleterious effects through activation of the DNA repair response [63,64] and activation of cellular senescence. [65] Epidemiologic studies have clearly associated telomere shortening with chronologic aging [66,67] and, perhaps more interestingly, it has been found that telomere shortening is accelerated by psychological stress. [68-71] Whether causative or solely a biomarker, these findings are exciting, and further research in this area is likely to shed light on these relationships in the next few years.
Proteostasis
Although damage and repair of DNA during aging have received considerable attention in the past, proteins are now sharing the limelight, based on the fact that proteins are responsible for actually carrying out most of the functions of a cell. Just as with other macromolecular damage, research has focused less on the source of damage and more on the mechanisms that control responses and preserve the health of the proteome. This includes quality control mechanisms, collectively termed proteostasis, which include mainly chaperones, autophagy, proteosomal degradations, and others, such as endoplasmic reticulum (ER) and mitochondrial unfolded protein responses (UPRs). [72-75] In addition to being implicated in the aging rate, at least in Caenorhabditis elegans, [76-78] proteostasis mechanisms have also been implicated in many age-related diseases, including neurodegeneration (e.g., Alzheimer, Parkinson diseases) and systemic diseases characterized by the accumulation of intracellular or extracellular protein aggregates. [79-81] Loss of proteostasis appears to play a double role in aging and related diseases. First, there is a general decline with age in the activity of several quality control pathways, including chaperone inducibility, autophagy, and proteasome functions. [76-78,82] In addition, there is an increased burden of damaged proteins that need to be considered as a result of accumulation of toxic aggregates and other entities. On the positive side, this means that the problems of protein aggregation can be attacked on two fronts—decrease the damage or increase the defenses. In the past, emphasis has been placed heavily on decreasing or precluding the damage (see earlier, “Macromolecular Damage’), but current efforts are shifting toward improving the defenses by activating otherwise depressed proteostasis pathways. Recent research suggests that the various protein quality control mechanisms can interact and compensate for each other, both within a given cell and, perhaps more exciting, even at a distance. [83,84] This might have important translational potential, because it might be possible to improve the entire system by intervening in focused (but yet to be determined) pathways and cells.
Stem Cells and Regeneration
The potential of stem cells as a panacea for all types of age-related diseases has been widely touted, especially in the media. However, these claims need to be tempered by a careful assessment of the possible roles of stem cells during aging and disease. The last decade has seen a set of elegant experiments using heterochronic parabiosis—the pairing of a young and old mouse so that the animals share a common circulatory system via a process called anastomosis—in which it has been shown that often the problem with aging resides less with the stem cells themselves, but rather with their niche and circulating activating factors. [85] Therefore, at least in the case of muscle [85] and perhaps the ovary, [86] stem cells are still present in older individuals, but their niche appears to be incapable of activating them. Further analyses have indicated the existence of circulating factors present in the serum of young mice, capable of activating stem cells in the tissue of the older parabiont partners, [87-89] as well as the opposite (factors in old serum capable of inhibiting stem cells in the younger animal). [90] It is crucial to gain a better understanding of stem cells and their niches in different tissues and their role (or not) in each age-related disease before rational therapeutic approaches can be devised. It might be easier to modify the niche than to inject actual young stem cells into old patients, which might not prove to be a useful strategy unless the aged niche can support the function of the injected young cells. Another exciting area of research in this area involves induced pluripotent stem cells (iPSCs), [91-93] which are already becoming important research tools, but might also have therapeutic potential (with the caveats described above for so-called standard young stem cells). This is a rapidly expanding field of research and much remains to be learned, both about stem cells in general and their aging characteristics and their possible roles in various age-related diseases.
Aging biology has undergone a revolutionary change in the last few decades, and there are many additional areas of exciting research that are not covered in the brief section just presented. Notable among them are rather recent findings from comparative biology [94-96] or the use of novel animal models. Similarly, no discussion was included about the notable contributions of classical evolutionary biology or demography, fields, which certainly shape the theoretical and conceptual contexts within which aging biology research is conducted. With the advent of multiple -omics technologies, comprehensive approaches such as systems biology are gaining attention, although thus far little of substance has been produced. [21]
– by Felipe Sierra, Ph.D. [Editor’s note: this article continues in additional sections.]
Geroscience Article Continues in 4 Sections
- Part 1 of 4: Introduction to the Geroscience essay on aging, and backgrounder on Sierra.
- Part 2 of 4: The Main Pillars of Research on Aging Biology (this article).
- Part 3 of 4: Geroscience (explains the field of geroscience and the importance of studying aging at the most basic biologic level).
- Part 4 of 4: A Tentative Look into the Future (ways geroscience hopes to increase life span).
Show Us Some Love
- Share this post on social media and help us spread the word– It only takes one click on any of the social media links on this page.
- Follow us on social media – Google+ or Reddit
- Sign up for our email list – We use your email to notify you of new articles. We will not send you spam, and we will not share your email address. You can cancel at any time.
- Tell us what you think of geroscience – Scroll down to enter your comments below.
References Accompanying this Section
(References provided by Dr. Felipe Sierra in Geroscience.)
14. Wheeler HE, Kim SK. Genetics and genomics of human aging. Philos Trans R Soc Lond B Biol Sci 366:43–50, 2011.
15. Kennedy BK, Berger SL, Brunet A, et al. Geroscience: linking aging to chronic disease. Cell 159:709–713, 2014.
16. López-Otín C, Blasco MA, Partridge L, et al. The hallmarks of aging. Cell 153:1194–1217, 2013.
17. Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its potential contribution to age-associated diseases. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S4–S9, 2014.
18. Epel E, Lithgow GJ. Stress biology and aging mechanisms: toward understanding the deep connection between adaptation to stress and longevity. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S10–S16, 2014.
19. Brunet A, Berger SL. Epigenetics of aging and aging-related disease. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S17–S20, 2014.
20. Newgard CB, Pessin JE. Recent progress in metabolic signaling pathways regulating aging and life span. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S21–S27, 2014.
21. Richardson AG, Schadt EE. The role of macromolecular damage in aging and age-related disease. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S28–S32, 2014.
22. Morimoto RI, Cuervo AM. Proteostasis and the aging proteome in health and disease. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S33–S38, 2014.
23. Rando TA, Wyss-Coray T. Stem cells as vehicles for youthful regeneration of aged tissues. J Gerontol A Biol Sci Med Sci 69(Suppl 1):S39–S42, 2014.
24. Howcroft TK, Campisi J, Louis GB, et al. The role of inflammation in age-related disease. Aging (Albany NY) 5:84–93, 2013.
25. Wang GC, Casolaro V. Immunologic changes in frail older adults. Transl Med UniSA 9:1–6, 2014.
26. Gomez CR, Acuña-Castillo C, Pérez C, et al. Diminished acute phase response and increased hepatic inflammation of aged rats in response to intraperitoneal injection of lipopolysaccharide. J Gerontol A Biol Sci Med Sci 63:1299–1306, 2008.
27. Jurgens HA, Johnson RW. Dysregulated neuronal-microglial crosstalk during aging, stress and inflammation. Exp Neurol 233:40–48, 2012.
28. De Martinis M, Franceschi C, Monti D, et al. Inflamm-ageing and lifelong antigenic load as major determinants of ageing rate and longevity. FEBS Lett 579:2035–2039, 2005.
29. Hsu FC, Kritchevsky SB, Liu Y, et al. Association between inflammatory components and physical function in the health, aging, and body composition study: a principal component analysis approach. J Gerontol A Biol Sci Med Sci 64:581–589, 2009.
30. Bruunsgaard H, Pedersen BK. Age-related inflammatory cytokines and disease. Immunol Allergy Clin North Am 23:15–39, 2003.
31. Bruunsgaard H, Andersen-Ranberg K, Hjelmborg JB, et al. Elevated levels of tumor necrosis factor alpha and mortality in centenarians. Am J Med 115:278–283, 2003.
32. McEwen BS. Brain on stress: how the social environment gets under the skin. Proc Natl Acad Sci U S A 109(Suppl 2):17180–17185, 2013.
33. Epel ES, Blackburn EH, Lin J, et al. Accelerated telomere shortening in response to life stress. Proc. Natl Acad Sci USA 101:17312–17315, 2004.
34. Aydinonat D, Penn DJ, Smith S, et al. Social isolation shortens telomeres in African grey parrots (Psittacus erithacus erithacus). PLoS ONE 9:e93839, 2014.
35. Zalli A, Carvalho LA, Lin J, et al. Shorter telomeres with high telomerase activity are associated with raised allostatic load and impoverished psychosocial resources. Proc Natl Acad Sci U S A 111:4519–4524, 2014.
36. Calabrese EJ, Iavicoli I, Calabrese V. Hormesis: why it is important to biogerontologists. Biogerontology 13:215–235, 2012.
37. Rando TA, Chang HY. Aging, rejuvenation, and epigenetic reprogramming: resetting the aging clock. Annu Rev Biochem 77:727–754, 2008.
38. Wood JG, Hillenmeyer S, Lawrence C, et al. Chromatin remodeling in the aging genome of Drosophila. Aging Cell 9:971–978, 2010.
39. Greer EL, Maures TJ, Ucar D, et al. Transgenerational epigenetic inheritance of longevity in Caenorhabditis elegans. Nature 479:365–371, 2011.
40. Kato M, Chen X, Inukai S, et al. Age-associated changes in expression of small, noncoding RNAs, including microRNAs, in C. elegans. RNA 17:1804–1820, 2011.
41. Imai SI, Guarente L. NAD+ and sirtuins in aging and disease. Trends Cell Biol 24:464–471, 2014.
42. Rehan L, Laszki-Szczachor K, Sobieszczanska M, et al. SIRT1 and NAD as regulators of ageing. Life Sci 105:1–6, 2014.
43. De Cabo R, Carmona-Gutierrez D, Bernier M, et al. The search for antiaging interventions: from elixirs to fasting regimens. Cell 157:1515–1526, 2014.
44. Baur JA, Pearson KJ, Price NL, et al. Resveratrol improves health and survival of mice on a high-calorie diet. Nature 444:337–342, 2006.
45. Pérez VI, Van Remmen H, Bokov A, et al. The overexpression of major antioxidant enzymes does not extend the lifespan of mice. Aging Cell 8:73–75, 2009.
46. Rea SL. Metabolism in the Caenorhabditis elegansMit mutants. Exp Gerontol 40:841–849, 2005.
47. Ristow M, Schmeisser S. Extending life span by increasing oxidative stress. Free Radic Biol Med 51:327–336, 2011.
48. Munkácsy E, Rea SL. The paradox of mitochondrial dysfunction and extended longevity. Exp Gerontol 56:221–233, 2014.
49. Man AL, Gicheva N, Nicoletti C. The impact of ageing on the intestinal epithelial barrier and immune system. Cell Immunol 289:112–118, 2014.
50. Heintz C, Mair W. You are what you host: microbiome modulation of the aging process. Cell 156:408–411, 2014.
51. Jenwitheesuk A, Nopparat C, Mukda S, et al. Melatonin regulates aging and neurodegeneration through energy metabolism, epigenetics, autophagy and circadian rhythm pathways. Int J Mol Sci 15:16848–16884, 2014.
52. Froy O. Circadian aspects of energy metabolism and aging. Ageing Res Rev 12:931–940, 2013.
53. Harman D. Aging: a theory based on free radical and radiation chemistry. J Gerontol 2:298–300, 1956.
54. Van Remmen H, Ikeno Y, Hamilton M, et al. Life-long reduction in MnSOD activity results in increased DNA damage and higher incidence of cancer but does not accelerate aging. Physiol Genomics 16:29–37, 2003.
55. Schriner SE, Linford NJ, Martin GM, et al. Extension of murine life span by overexpression of catalase targeted to mitochondria. Science 308:1909–1911, 2005.
56. Pala FS, Gürkan H. The role of free radicals in ethiopathogenesis of diseases. Adv Molec Biol 1:1-9, 2008.
57. Trifunovic A, Wredenberg A, Falkenberg M, et al. Premature ageing in mice expressing defective mitochondrial DNA polymerase. Nature 429:417–423, 2004.
58. Wallace DC. A mitochondrial paradigm of metabolic and degenerative diseases, aging, and cancer: a dawn for evolutionary medicine. Annu Rev Genet 39:359–407, 2005.
59. Hoeijmakers JH. DNA damage, aging, and cancer. N Engl J Med 361:1475–1485, 2009.
60. Rodríguez S, Eriksson M. Evidence for the involvement of lamins in aging. Curr Aging Sci 3:81–89, 2010.
61. Worman HJ. Nuclear lamins and laminopathies. J Pathol 226:316–325, 2012.
62. Sierra F. Is (your cellular response to) stress killing you? J Gerontol A Biol Sci Med Sci 61:557–561, 2006.
63. Collado M, Blasco MA, Serrano M. Cellular senescence in cancer and aging. Cell 130:223–233, 2007.
64. Shay JW, Wright WE. Senescence and immortalization: role of telomeres and telomerase. Carcinogenesis 26:867–874, 2005.
65. Bodnar AG, Ouellette M, Frolkis M, et al. Extension of life-span by introduction of telomerase into normal human cells. Science 279:349–352, 1998.
66. Cawthon RM, Smith KR, O’Brien E, et al. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet 361:393–395, 2003.
67. Epel ES, Merkin SS, Cawthon R, et al. The rate of leukocyte telomere shortening predicts mortality from cardiovascular disease in elderly men. Aging (Albany, NY) 1:81–88, 2009.
68. Quinlan J, Tu MT, Langlois EV, et al. Protocol for a systematic review of the association between chronic stress during the life course and telomere length. Syst Rev 3:40–47, 2014.
69. Blasco MA. Telomere length, stem cells and aging. Nat Chem Biol 3:640–649, 2007.
70. Herrera E, Samper E, Martín-Caballero J, et al. Disease states associated with telomerase deficiency appear earlier in mice with short telomeres. EMBO J 18:2950–2960, 1999.
71. Parks CG, Miller DB, McCanlies EC, et al. Telomere length, current perceived stress, and urinary stress hormones in women. Cancer Epidemiol Biomarkers Prev 18:551–560, 2009.
72. Cuervo AM, Wong E. Chaperone-mediated autophagy: roles in disease and aging. Cell Res 24:92–104, 2014.
73. Cuervo AM. Autophagy and aging: keeping that old broom working. Trends Genet 24:604–612, 2008.
74. Jankowska E, Stoj J, Karpowicz P, et al. The proteasome in health and disease. Curr Pharm Des 19:1010–1028, 2013.
75. Lionaki E, Tavernarakis N. Oxidative stress and mitochondrial protein quality control in aging. J Proteomics 92:181–194, 2013.
76. Morley JF, Morimoto RI. Regulation of longevity in Caenorhabditis elegansby heat shock factor and molecular chaperones. Mol Biol Cell 15:657–664, 2004.
77. Dillin A, Cohen E. Ageing and protein aggregation-mediated disorders: from invertebrates to mammals. Philos Trans R Soc Lond B Biol Sci 366:94–98, 2011.
78. Hsu AL, Murphy CT, Kenyon C. Regulation of aging and agerelated disease by DAF-16 and heat-shock factor. Science 300:1142–1145, 2003.
79. Powers ET, Morimoto RI, Dillin A, et al. Biologic and chemical approaches to diseases of proteostasis deficiency. Annu Rev Biochem 78:959–991, 2009.
80. Kakizuka A. Protein precipitation: a common etiology in neurodegenerative disorders? Trends Genet 14:396–402, 1998.
81. Stefani M, Dobson CM. Protein aggregation and aggregate toxicity: new insights into protein folding, misfolding diseases and biologic evolution. J Mol Med (Berl) 81:678–699, 2003.
82. Koga H, Kaushik S, Cuervo AM. Protein homeostasis and aging: the importance of exquisite quality control. Ageing Res Rev 10:205–215, 2011.
83. Wong E, Cuervo AM. Integration of clearance mechanisms: the proteasome and autophagy. Cold Spring Harb Perspect Biol 2:a006734, 2010.
84. Dillin A, Gottschling DE, Nyström T. The good and the bad of being connected: the integrons of aging. Curr Opin Cell Biol 26:107–112, 2014.
85. Conboy IM, Conboy MJ, Wagers AJ, et al. Rejuvenation of aged progenitor cells by exposure to a young systemic environment. Nature 433:760–764, 2005.
86. Woods DC, Tilly JL. An evolutionary perspective on adult female germline stem cell function from flies to humans. Semin Reprod Med 31:24–32, 2013.
87. Loffredo FS, Steinhauser ML, Jay SM, et al. Growth differentiation factor 11 is a circulating factor that reverses age-related cardiac hypertrophy. Cell 153:828–839, 2013.
88. Katsimpardi L, Litterman NK, Schein PA, et al. Vascular and neurogenic rejuvenation of the aging mouse brain by young systemic factors. Science 344:630–634, 2014.
89. Villeda SA, Plambeck KE, Middeldorp J, et al. Young blood reverses age-related impairments in cognitive function and synaptic plasticity in mice. Nat Med 20:659–663, 2014.
90. Villeda SA, Luo J, Mosher KI, et al. The ageing systemic milieu negatively regulates neurogenesis and cognitive function. Nature 477:90–94, 2011.
91. Liu GH, Ding Z, Izpisua Belmonte JC. iPSC technology to study human aging and aging-related disorders. Curr Opin Cell Biol 24:765–774, 2012. [Link to article.]
92. Mahmoudi S, Brunet A. Aging and reprogramming: a two-way street. Curr Opin Cell Biol 24:744–756, 2012.
93. Isobe KI, Cheng Z, Nishio N, et al. iPSCs, aging and age-related diseases. N Biotechnol 31:411–421, 2014.
94. Austad SN. Comparative biology of aging. J Gerontol A Biol Sci Med Sci 64:199–201, 2009.
95. Miller RA, Williams JB, Kiklevich JV, et al. Comparative cellular biogerontology: primer and prospectus. Ageing Res Rev 10:181–190, 2011.
96. Gorbunova V, Seluanov A, Zhang Z, et al. Comparative genetics of longevity and cancer: insights from long-lived rodents. Nat Rev Genet 15:531–540, 2014.
References
Cover photo credit: Sebastian Kaulitzki / Shutterstock.
National Institute on Aging. “Felipe Sierra.” National Institutes of Health. Web, Retrieved 10 Jan 2018. Link to Article.
Felipe Sierra. “Geroscience.” Brocklehurst’s Textbook of Geriatric Medicine and Gerontology, 8th Edition, Authors: Howard Fillit Kenneth Rockwood John B Young. ISBN: 978-0-7020-6185-1
Disclaimer
Diagnosis, Treatment, and Advice: This article is intended for educational and informational purposes only and is not a substitute for qualified, professional medical advice. The information and opinions provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. Consult a qualified and licensed physician for the diagnosis and treatment of any and all medical conditions. Experimental therapies carry a much higher risk than FDA-approved ones. Call 911, or an equivalent emergency hotline number, for all medical emergencies. As well, consult a licensed, qualified physician before changing your diet, supplement or exercise programs.
Photos, Endorsements, & External Links: This article is not intended to endorse organizations, companies, or their products. Links to external websites, mention or depiction of company names or brands, are intended for illustration only and do not constitute endorsements.
3 Replies to “Main Pillars of Research in Revolutionary Geroscience Field”
Comments are closed.